Analysis of its client portfolio from leading independent employee benefits consultancy Broadstone demonstrates the recent growth in Private Medical Insurance (PMI) claims incidence. The proportion of members insured on PMI that have made a claim – the claims incidence – has risen from 21% in 2021 to 27% in 2024, a six percentage point increase.
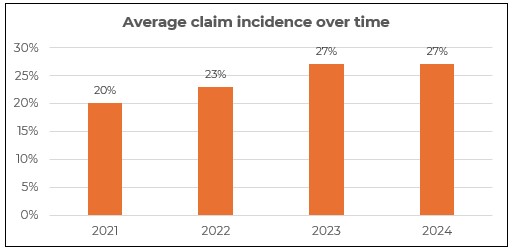
It demonstrates the impact of increased strain on the NHS following the pandemic and reduced access to primary care pushing patients towards the private sector to receive timely treatment.
Sharon Harwood-Davis, Head of Corporate Healthcare Pricing at Broadstone, said: “The jump in growth of PMI claims since 2021 is a clear indicator of an NHS that is struggling to meet demand. Employers recognise the importance of putting in place healthcare provision for their employees and their families to reduce sickness absence costs and help maintain productivity. Since lockdown, we have seen organisations broaden the eligibility criteria within the workplace and workers are increasingly taking advantage of the increased access to the private sector. Businesses need to understand, however, that the rise in the frequency of claims is likely to directly drive premium inflation from insurers. Understanding the drivers behind the claims experience is becoming increasingly important. Only through this data-driven approach can sensible mechanisms be put in place to help employers manage the longer-term cost sustainability of funding Private Healthcare benefits.”
The data suggests that spending on cancer claims, as a percentage of total claims spend, has stabilised after a surge in people coming forward for diagnostics and treatment following the pandemic.
Musculoskeletal conditions account for the highest proportion of spend (39% in 2025 YTD) and that proportion has remained relatively constant for a number of years.
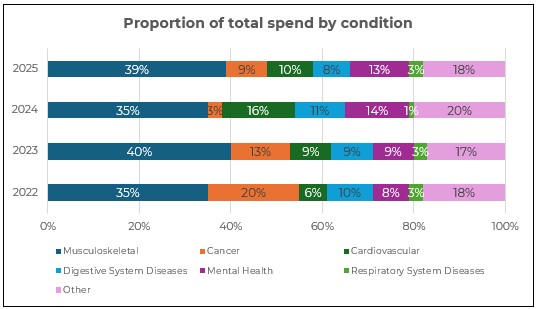
However, the data shows a sharp rise in the proportion spent on mental health claims through PMI products – increasing from 8% in 2022 to 13% in 2025 YTD. In contrast, the proportion of claims cost spent on cancer treatments has fallen significantly from 20% in 2022 to 9% in 2025 YTD.
Sharon Harwood-Davis added: “One of the most striking shifts we are seeing is the sharp increase in demand for mental health support through PMI. This reflects both a positive cultural shift, with more employees willing to seek help, and practical pressures, with long NHS waiting lists pushing individuals to use PMI cover to access counselling, CBT and psychiatric care. Mental health support is no longer a peripheral add-on; it has become a central feature of workplace healthcare provision and must be planned for accordingly. It is becoming increasingly essential for organisations to review what can be done to not only support ongoing mental health concerns but also to implement robust preventative solutions to support employees and their families before active treatment is required.”
|

